Background
The natural killer (NK) cells, defined by CD56 or CD16 expression and the absence of CD3, are a kind of lymphocytes that can remove virus-infected cells as well as cancer cells by immunologic processes without prior sensitization. Activated NK cells can release cytokines such as IFN-γ that play an essential role in the activation and regulation of both adaptive and innate immunity. The use of allogeneic NK cells allows the selection of donor NK cells from non-HLA-related healthy donors with higher flexibility, which enables to manufacture large amount of expanded and cryopreserved cells for off-the-shelf use. In this study, we explored the safety and efficacy of MG4101, ex vivo-expanded allogeneic NK cells in combination with rituximab, anti-CD20 monoclonal antibody in relapsed or refractory non-Hodgkin lymphoma (NHL) patients.
Methods
In this open-label, multi-center, phase 1 study (NCT03778619), dose escalation was conducted according to a 3+3 design with three dose levels of MG4101 (1X107 cells/kg, 3X107 cells/kg and 9X107 cells/kg). MG4101 and IL-2 (1X106 IU/m2, sc) were administered every two weeks for 6 cycles. Patients received lymphodepleting chemotherapy of fludarabine 20mg/m2/day and cyclophosphamide 250mg/m2/day for three days before the administration of MG4101 at cycle 1, 3, and 5. Patients also received rituximab 375mg/m2 every two weeks during the first 2 cycles and then every four weeks until 6th cycle. After completion of the cycle 6, additional treatment was allowed for up to 8 cycles according to investigator's discretion. The primary objective of the study was to determine the maximum tolerated dose (MTD) and the secondary objectives include efficacy, immunological assays, and pharmacokinetics.
Results
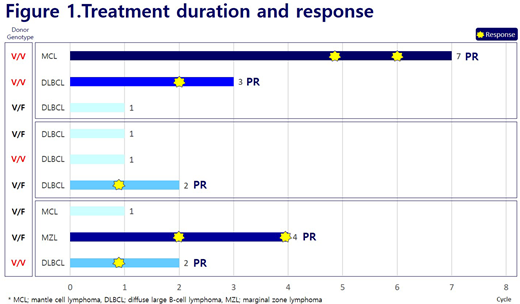
A total of nine patients (6 diffuse large B-cell lymphoma (DLBCL), 2 mantle cell lymphoma (MCL), and one marginal zone lymphoma (MZL)) were enrolled in the study. The median age was 64 years (range 38-80). The median number of prior systemic therapies was four (range 2-6) which had to include at least one regimen of rituximab-containing treatment. The median number of administered cycles was two (range 1-7). Most adverse events (AEs) were primarily grade 1/2 and did not require dose delays. Grade ≥ 3 AEs occurred in seven patients (7/9, 77.8%), of which five (5/9, 55.6%) were considered treatment-related. The most frequent grade ≥ 3 AEs were neutropenia (5/9, 55.6%), febrile neutropenia (2/9, 22.2%), and other AEs were reported in each individual patient with thrombocytopenia, anemia, pneumonia, decreased appetite, hypokalaemia, hypotension, or tumor hemorrhage, respectively. Most of hematologic toxicities were observed after lymphodepleting chemotherapy. Serious treatment-related AEs in two patients were fever (2/9, 22.2%) suspected to be grade 1 cytokine-release syndrome, and all patients recovered in a week. None experienced dose-limiting toxicities (DLTs); maximal tolerated dose (MTD) was not reached. The objective response rate was 55.6% with five partial responses (DLBCL 3, MCL 1, MZL 1; Figure 1). MG4101 was found to persist for up to 14 days by a nested polymerase chain reaction (PCR) assay. Donor specific antibodies have been detected in one patient with ≤ 2,000 mean fluorescence intensity (MFI), but there was no graft-versus-host disease (GvHD).
Conclusion
The combination therapy of MG4101 with rituximab is a very tolerable treatment with an encouraging antitumor effect in relapsed or refractory NHL patients with a 55.6% response rate. The updated immunological profile, cytokine production, and survival data will be presented.
Yoon:Amgen, Chongkundang, Celgene, Astrazeneca: Consultancy; Samyang: Research Funding; Celltrion: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal